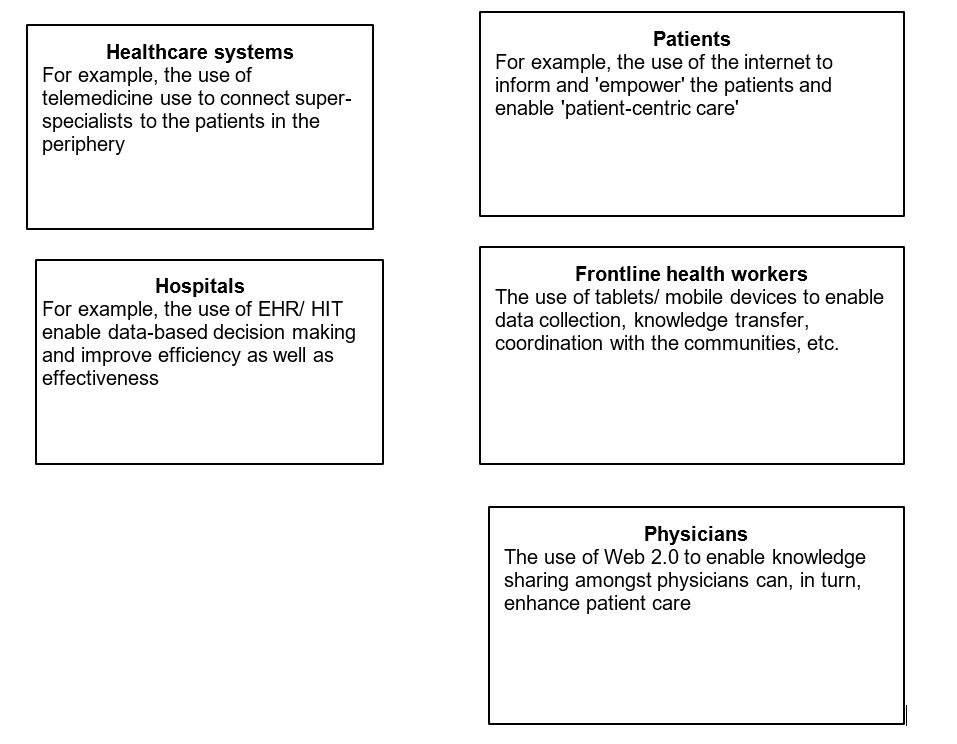
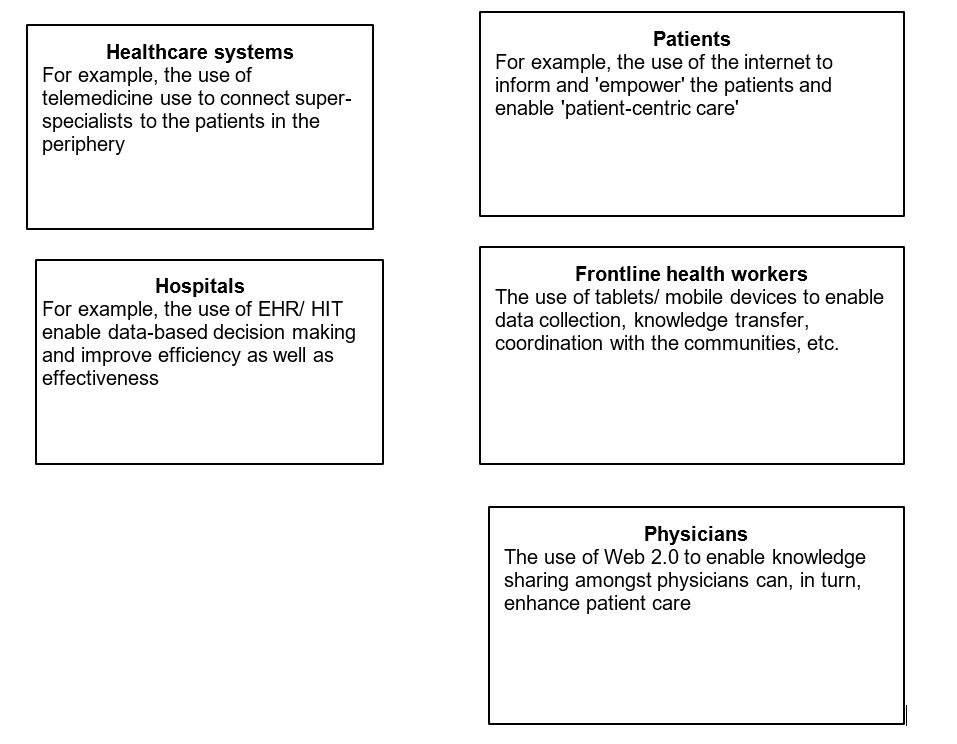
Information and Communication Technologies (ICT) can play a significant role in enhancing healthcare delivery and have a range of implications for various stakeholders-healthcare providers, service seekers, hospitals and hospital systems, and governments (Nicolini et al., 2008). To understand these, two views have been proposed. A deterministic view of ICT (Wyatt, 2008) entails conceptualizing technology as 'objective' where appropriate design, and implementation of ICT can enhance patient care (Figure).
Figure: The implications of IT for diverse stakeholders in healthcare
However, the human aspect of technology makes it imperative to take into account the socio-cultural aspects of 'health' in general and the complex relationships among the stakeholders in particular (Orlikowski, 1992). This view highlights the significance of taking an embedded and contextual (Jones & Karsten, 2008) perspective of ICT in healthcare and of in-depth studies to uncover the dynamics involved. It is these embedded dynamics that result in formulation and implementation gaps in many of the ICT initiatives in healthcare. The paragraphs below outline my understanding of the implications for stakeholders based on selected field-based studies.1
Enhancing healthcare systems through telemedicine
Potentially, telemedicine can enhance the accessibility, affordability, and quality of healthcare services in India, and bridge the rural-urban divide in healthcare. In the recent pandemic, telemedicine emerged as an important mode of healthcare delivery across the nation. In March 2020, the central Government cleared the long-pending regulatory hurdle to telemedicine by drafting guidelines for enabling telemedicine practice. Sustainable scaling-up of telemedicine requires addressing infrastructural, human resource, and socio-cultural issues, apart from strengthening the policy/regulatory aspects (Chandwani & Dwivedi, 2015). Specifically, the human factors in any technology intervention are important determinants of successful implementation. For example, in one study we analyzed the doctor-patient interactions over telemedicine from the perspective of two intersecting institutional logics in health IT, namely logic of care and logic of choice. We found that though telemedicine provided a choice to the patients, thus emphasizing the logic of choice, the patient accepted telemedicine only when the design was modified to enhance the perception of the care logic (Chandwani & De, 2017). In another study, we took a systems view of telemedicine. We conceptualized telemedicine as connectivity among nodes rather than between doctor and patients alone, thus highlighting the scope of increased flow of clinical, managerial, and technological information among the nodes, and the use of both online and offline communication (Chandwani et al., 2018). We also noted the importance of learning and skill development of the local doctor, and of molding naive patients into expert patients, both in technology use and self-management of disease (Chandwani et al., 2018). In another study, invoking the lenses of human infrastructure and seamful spaces, we highlight the role of engaging the human actors-coordinators, local doctors, and patients themselves - in implementing telemedicine as a co-creation process (Chandwani & Kumar, 2018).
Implications for healthcare systems and hospitals
The above studies highlight the critical role of the human factor and its interaction with technology and practices in determining the successful implementation of health IT. Overcoming health IT resistance entails understanding contextual nuances of healthcare through a conceptual framework that includes people, practice, and technology (Kumar et al., 2020). Our review shows that the framework is useful in understanding the power dynamics within the healthcare system/ organization (Kumar et al 2020). In an ongoing study, we invoke a Bourdeausian perspective to analyze resistance to EHR implementation in a large multispecialty hospital. The initial findings highlight the role of emotional capital in a doctor's practice as an important determinant of resistance.
The following paragraphs highlight how technology affects specific actors in healthcare: patients, frontline health workers, and doctors.
Patients
In the recent past, the focus on patient empowerment (Anderson & Funnell, 2010) has emphasized participatory decision making between the doctor and the patient. The internet, with its wide penetration, can help patients or their relatives acquire the knowledge needed to participate in an 'informed' decision making process. However, while most of the research on the role of the internet in physician-patient interaction paints a fairly optimistic view of this phenomenon, our study highlighted its effect on the traditional power relationship between doctors and patients in the Indian context (Chandwani & Kulkarni, 2016). The existing structures, norms and beliefs about the physician-patient relationship played a critical role in actors ascribing distinct meanings to the phenomenon of 'internet informed patients'. In another study, we investigate the health information-seeking behavior and dietary choices of diabetic patients in India. We highlight how the broader social network of friends, family, and acquaintances shapes individual beliefs about diabetes and how cultural aspects influence dietary decisions (Hentschel et al., 2017).
Frontline health workers
Frontline health workers such as ASHAs (Accredited Social Health Activists) and Anganwadi workers form the backbone of rural healthcare delivery in India. Several studies have highlighted the use of m-health for enhancing the work of frontline healthcare workers (Chib, 2010). In our study with ASHAs, we found that m-health interventions were useful in enhancing breast cancer awareness amongst rural women (Fletcher-Brown et al., 2020). The study also highlighted how the ASHAs used the technology to address some norms about knowledge seeking amongst rural women in general and socio-cultural beliefs about breast cancer in particular. In ongoing research, we are investigating the socio-psychological aspects of ICT use by the frontline workers and trying to explore whether and how it affects the fundamental identity of ASHAs.
Physicians
Several studies have highlighted the use of Web 2.0 by physicians to upgrade their knowledge and to enhance the quality of care delivered to patients (Sims, 2018). Prior literature, however, has examined the knowledge sharing and knowledge seeking factors separately. In our study, we examined the effect of both seeking and sharing factors in an integrated model (Singh et al., 2018). The study revealed that knowledge sharing factors are more important for the use of Web 2.0 and that self-efficacy and enjoyment of sharing knowledge are important determinants of sharing rather than reciprocity. In another study, we found that reputation and face concern (concern to create a positive social image) moderated the relationship between attitude and intention to share knowledge (Maheshwari et al., 2020). The findings highlight the contextual understanding of physician position and role in the healthcare system.
To summarize, the above studies dwell on the human factors involved in the implementation of ICT initiatives in healthcare. The studies problematize the deterministic and simplistic view of technology and emphasize a contextual and nuanced understanding of the phenomenon.
References
Chandwani, R. K., & Dwivedi, Y. K. (2015). Telemedicine in India: Current state, challenges, and opportunities. Transforming Government: People, Process, and Policy.
Chandwani, R., & Kulkarni, V. (2016, May). Who's the Doctor? Physicians' Perception of Internet Informed Patients in India. In Proceedings of the 2016 CHI Conference on Human Factors in Computing Systems (pp. 3091-3102).
Chandwani, R., & Kumar, N. (2018, April). Stitching Infrastructures to Facilitate Telemedicine for Low-Resource Environments. In Proceedings of the 2018 CHI Conference on Human Factors in Computing Systems (pp. 1-12).
Chandwani, R., and De, R. (2017). Doctor-patient interaction in telemedicine: Logic of choice and logic of care perspectives. Information Systems Frontiers, 19(4), 955-968.
Chandwani, R., De, R., & Dwivedi, Y. K. (2018). Telemedicine for low resource settings: Exploring the generative mechanisms. Technological forecasting and social change, 127, 177-187.
Fletcher-Brown, J., Carter, D., Pereira, V., & Chandwani, R. (2020). Mobile technology to give a resource-based knowledge management advantage to community health nurses in an emerging economies context. Journal of Knowledge Management..
Hentschel, J., Sherugar, S. M., Zhou, R., Kameswaran, V., Chandwani, R., & Kumar, N. (2017, May). Rice Today, Roti Tomorrow: Diets and Diabetes in Urban Indian Households. In Proceedings of the 2017 CHI Conference on Human Factors in Computing Systems (pp. 4069-4081).
Jones, M. R., & Karsten, H. (2008). Giddens's structuration theory and information systems research. MIS Quarterly, 32(1), 127-157.
Kumar, M., Singh, J. B., Chandwani, R., & Gupta, A. (2020). "Context" in healthcare information technology resistance: A systematic review of extant literature and agenda for future research. International Journal of Information Management, 51, 102044.
Maheshwari, B., Sarrion, M., Motiani, M., O'Sullivan, S., & Chandwani, R. (2020). Exploration of factors affecting the use of Web 2.0 for knowledge sharing among healthcare professionals: An Indian perspective. Journal of Knowledge Management.
Orlikowski, W. J. (1992). The duality of technology: Rethinking the concept of technology in organizations. Organization science, 3(3), 398-427.
Singh, J. B., Chandwani, R., & Kumar, M. (2018). Factors affecting Web 2.0 adoption: exploring the knowledge sharing and knowledge-seeking aspects in health care professionals. Journal of Knowledge Management.
Wyatt, S. (2008). Technological determinism is dead; long live technological determinism. The handbook of science and technology studies, 3, 165-180.
1The purpose is not to provide an extensive review of ICT interventions in healthcare but to emphasize the in-depth understanding of the phenomenon based on these studies.
About The Author
Prof Rajesh Chandwani
Rajesh Chandwani is an associate professor in the Human Resources Management area.